6 Common Autoimmune Diseases
Understanding their symptoms, causes, and treatment
Please note that these summaries offer a general overview of autoimmune diseases, and each condition can vary in terms of symptoms, severity, and treatment approaches. Consulting with healthcare professionals is essential for accurate diagnosis and personalized management.
-
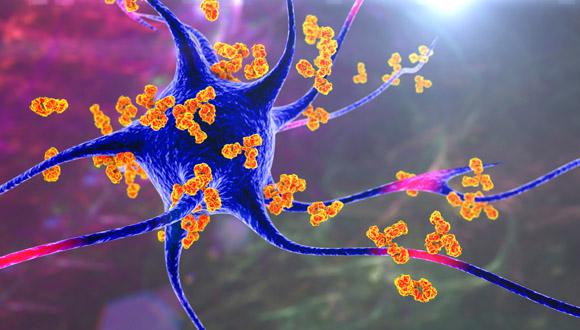
Rheumatoid Arthritis (RA):
- RA is a chronic inflammatory disorder that primarily affects the joints.
- The immune system mistakenly attacks the body's own tissues, particularly the synovium, which is the lining of the joints. leading to joint pain, stiffness, swelling in the affected joints.
- RA typically affects the smaller joints first, such as those in the hands and feet, but it can progress to involve larger joints as well. The joints may become tender to the touch, and the inflammation can lead to joint deformity and limited range of motion.
- It can also affect other organs, such as the heart, lungs, and eyes.
- The exact cause of RA is not fully understood, but it is believed to involve a combination of genetic and environmental factors. Women are more commonly affected by RA than men.
- Treatment involves medication to reduce inflammation and manage symptoms, slow down the progression of joint damage, and improve overall quality of life.
-
Systemic Lupus Erythematosus (SLE):
- SLE is a complex autoimmune disease that can affect multiple organs and systems, including the skin, joints, kidneys, heart, and brain.
- SLE is characterized by a wide range of symptoms that can vary from person to person. Common symptoms include fatigue, joint pain, skin rashes, fever, and organ involvement.
- The exact cause of SLE is unknown, but it is believed to involve a combination of genetic, environmental, and hormonal factors. As many other autoimmune diseases, it primarily affects women, with most cases occurring in women of childbearing age.
- Diagnosing SLE can be challenging, as its symptoms can mimic those of other conditions. Healthcare professionals rely on a combination of medical history, physical examination, blood tests, and imaging studies to make an accurate diagnosis.
- Treatment involves medications to manage symptoms and suppress the immune system, as well as lifestyle changes to minimize triggers and protect against organ damage.
-
Multiple Sclerosis (MS):
- MS is a chronic autoimmune disease that affects the central nervous system (CSN), including the brain and spinal cord.
- The immune system attacks the protective covering of nerve fibers called myelin, resulting in inflammation and damage, leading to communication problems between the brain and the rest of the body.
- The damage to the myelin disrupts the normal flow of electrical impulses along the nerve fibers, leading to a wide range of symptoms that can vary greatly from person to person, but often include fatigue, difficulty walking, numbness or tingling, muscle weakness, and problems with coordination and balance, problems with memory and concentration.
- MS can be categorized into different types, including relapsing-remitting MS (RRMS), secondary progressive MS (SPMS), primary progressive MS (PPMS), and progressive-relapsing MS (PRMS). These categories describe the course of the disease and how symptoms may evolve over time.
- There is currently no cure for MS, treatment aims to manage symptoms, slow the progression of the disease, and improve quality of life. Treatment options for MS include disease-modifying therapies (DMTs), which can reduce the frequency and severity of relapses and delay the accumulation of disability.
-
Type 1 Diabetes (T1D):
- T1D is also known as insulin-dependent diabetes or juvenile diabetes. It is a chronic autoimmune disease in which the immune system attacks and destroys the insulin-producing cells in the pancreas.
- As a result, the body cannot regulate blood sugar levels, leading to high blood sugar and a range of symptoms like increased thirst, frequent urination, weight loss, and fatigue. If left untreated, T1D can lead to serious complications, including cardiovascular disease, kidney damage, nerve damage, and eye problems.
- T1D usually develops in childhood or adolescence, but it can occur at any age.
- Treatment involves lifelong insulin therapy1, blood sugar monitoring, healthy eating, regular exercise, and education on managing the disease.
- Ongoing research is focused on improving treatment options and finding ways to prevent or halt the autoimmune destruction of beta cells.
-
Celiac Disease:
- Celiac disease is an autoimmune disorder triggered by the ingestion of gluten, a protein found in wheat, barley, and rye.
- The immune system responds to gluten by damaging the small intestine's lining, leading to malabsorption of nutrients and various symptoms.
- Common symptoms include digestive issues, fatigue, weight loss, and skin rashes.
- The only effective treatment is strict adherence to a gluten-free diet, which allows the intestine to heal and prevents further complications.
-
Psoriasis:
- Psoriasis is a chronic autoimmune skin disease characterized by the rapid buildup of skin cells, resulting in thick, red patches covered with silvery scales.
- The immune system mistakenly triggers an inflammatory response, causing the excessive growth of skin cells.
- Symptoms can range from mild to severe and may include itching, pain, and cracking of the skin.
- The most common type of psoriasis is called plaque psoriasis, which presents as raised, red patches of skin covered with silvery scales. Other types include guttate psoriasis (small, drop-like lesions), inverse psoriasis (affecting skin folds), pustular psoriasis (pus-filled blisters), and erythrodermic psoriasis (widespread inflammation).
- Treatment options include topical medications, phototherapy, systemic medications, biological drugs biologic drugs that target specific parts of the immune system., and lifestyle changes to manage symptoms and prevent flare-ups.
1 Jakubowicz, D., Landau, Z., Tsameret, S., et al (2019). Reduction in Glycated Hemoglobin and Daily Insulin Dose Alongside Circadian Clock Upregulation in Patients With Type 2 Diabetes Consuming a Three-Meal Diet: A Randomized Clinical Trial. Diabetes Care.