Sex, Gender and Autoimmunity
Understanding the influence of sex and gender on Autoimmunity
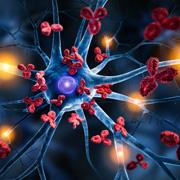
Autoimmunity is a complex and multifaceted phenomenon that occurs when the immune system mistakenly targets and attacks the body's own cells and tissues. While the exact mechanisms triggering autoimmunity are not fully understood, researchers have observed gender disparities in the prevalence, severity, and manifestations of autoimmune diseases. This intersection between autoimmunity and gender sheds light on the intricate interplay between genetics, hormones, and environmental factors.
Women are disproportionately affected by autoimmune diseases, with a higher incidence compared to men (78% of the autoimmune patients are woman). This pattern is evident across a spectrum of autoimmune conditions, raising questions about the role of gender-specific factors in the development and progression of these diseases.
One prominent factor contributing to the gender bias in autoimmunity is the role of sex hormones, particularly estrogen and testosterone. These hormones play a crucial role in regulating the immune system, influencing the activation and function of immune cells. Estrogen, for instance, has been shown to enhance certain aspects of the immune response, potentially contributing to an increased risk of autoimmunity in women. On the other hand, testosterone appears to have immunosuppressive effects, which might provide a protective effect against autoimmune diseases in men.
The influence of sex hormones on autoimmunity is exemplified by the fact that many autoimmune diseases exhibit a peak in incidence during the reproductive years, a period characterized by hormonal fluctuations. Conditions like rheumatoid arthritis and systemic lupus erythematosus often manifest or worsen during pregnancy or shortly after childbirth, when estrogen levels are high. Conversely, diseases such as ankylosing spondylitis and multiple sclerosis may show a later onset or reduced severity in men, possibly due to the protective effects of testosterone.
In addition to hormonal influences, genetic factors also contribute to the gender disparity in autoimmune diseases. Certain autoimmune conditions have been linked to specific genetic markers, and some of these markers show a gender-specific association. For example, specific human leukocyte antigen (HLA) alleles are implicated in the susceptibility to autoimmune diseases, and the prevalence of these alleles may vary between men and women. This suggests that genetic predisposition, combined with hormonal influences, creates a unique risk profile for autoimmunity in each gender.
The immune response itself may also be modulated by gender-specific differences in the expression of immune-related genes. Studies have identified sex-specific variations in the activity of immune cells and production of cytokines which regulate the immune responses. These differences may contribute to variations in the susceptibility, severity, and clinical presentation of the diseases between men and women.
Beyond hormonal and genetic factors, environmental factors can play a crucial role in shaping the gender-specific patterns of autoimmunity. Environmental triggers, such as infections, exposure to certain chemicals, as well as lifestyle factors, can interact with genetic predisposition and hormonal influences to initiate or exacerbate autoimmune responses. The impact of these environmental factors may vary between genders, further contributing to the observed gender disparities in autoimmune diseases.
The clinical manifestations of autoimmune diseases also exhibit gender-specific patterns. For instance, women with autoimmune diseases may experience more severe symptoms during certain phases of the menstrual cycle, pregnancy, or menopause. The influence of hormones on disease activity and the interaction between hormonal changes and the immune system contribute to these variations in symptoms.
Moreover, different autoimmune diseases predominantly affect one gender over the other. For example, autoimmune thyroid diseases like Hashimoto's thyroiditis and Graves' disease are more prevalent in women, while ankylosing spondylitis, a type of inflammatory arthritis, is more common in men. These gender-specific patterns suggest that there are unique underlying mechanisms driving autoimmunity in each gender.
In conclusion, the intersection between autoimmunity and gender is a captivating and complex which underscore the need for a comprehensive and gender-sensitive approach to research, diagnosis, and treatment. Researchers of the TAU Colton Center work to decipher the molecular and cellular mechanisms that contribute to gender-specific patterns in autoimmunity. We aim to assist researchers and clinicians to develop effective strategies for the prevention, early detection, and management of autoimmune diseases and, ultimately, improve the lives of patientes.
Reference: Sex and gender influence on immunity and autoimmunity/ Robert G Lahita
Top of Form