What the MICROBIOME GUT to do with it?
The connection between gut microbiome and autoimmune diseases
The relationship between the gut microbiome and autoimmune diseases has emerged as a pivotal area of biomedical research. Accumulating evidence suggests that the composition of gut bacteria not only influences the immune system but can also play a critical role in the onset and progression of autoimmune disorders.
The gut microbiome is a complex community of microorganisms—including bacteria, viruses, fungi, and protozoa—that live primarily in the large intestine. Collectively, microbial cells in the human body are estimated to rival or outnumber human cells, making the microbiome integral to health and disease. The roles of the gut microbiota include:
- Digesting dietary components not accessible to human enzymes.
- Synthesizing essential vitamins and bioactive compounds.
- Defending against pathogens by competing for resources and space.
- Regulating the immune system.
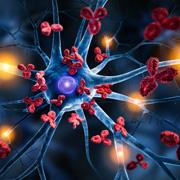
Both the innate and adaptive branches of the immune system are deeply influenced by the microbiome.
- The gut-associated lymphoid tissue (GALT)—including immune cells in the gut wall and mesenteric lymph nodes—constantly interfaces with microbial products.
- Microbial metabolites such as short-chain fatty acids (SCFAs) act as signaling molecules, influencing immune cell differentiation and inflammatory pathways.
- The microbiome modulates T cell populations, including T-helper (Th1, Th2, Th17) and regulatory T cells (Tregs), directly shaping responses to antigens.
- These regulatory effects extend systemically, affecting distal immune sites and influencing susceptibility to infections and inflammatory disease.
A healthy gut microbiome helps maintain the integrity of the intestinal barrier. This barrier restricts the passage of harmful antigens into the bloodstream. Disruption, often termed dysbiosis, can:
- Lead to increased intestinal permeability (“leaky gut”), allowing microbial products (such as lipopolysaccharide, LPS) and dietary antigens to reach immune cells, triggering inflammation.
- Compromise oral tolerance—a process by which the immune system is trained to ignore harmless antigens—making the body more susceptible to autoreactive immune responses.
Autoimmune diseases arise when the immune system mistakenly attacks the body’s own tissues, leading to conditions such as rheumatoid arthritis, multiple sclerosis, and type 1 diabetes. The etiology involves genetic susceptibility, environmental triggers, and increasingly, the composition and function of the gut microbiota.
Dysbiosis and Autoimmunity
Dysbiosis—an imbalance in gut microbiota diversity or function—has been consistently correlated with various autoimmune diseases. Main mechanisms by which dysbiosis may contribute include:
- Loss of microbial diversity: Reduced abundance of beneficial taxa and overgrowth of potentially harmful ones, often linked with increased inflammation and impaired immune modulation.
- Altered metabolite production: Changes in SCFA levels and other metabolites can reduce the pool of regulatory immune cells and favor pro-inflammatory states.
- Antigenic mimicry: Some microbial antigens resemble self-tissues (molecular mimicry), potentially prompting the immune system to attack host cells.
- Microbiota-induced inflammatory signaling: Dysregulated signaling via toll-like receptors (TLRs), nucleotide-binding oligomerization domain (NOD)-like receptors, and other pathways can amplify immune activation and break tolerance.
- Barrier dysfunction: As previously noted, increased permeability allows foreign and self-antigens to stimulate systemic immune responses, sustaining chronic inflammation.
The gut microbiome is central to maintaining immune tolerance and preventing autoimmunity. Dysbiosis—an imbalance of gut microbial communities—not only disrupts the mucosal barrier and local immune responses but also triggers and perpetuates autoimmune diseases systemically. A deeper understanding of these interactions is unlocking new preventive and therapeutic possibilities, including dietary modification, targeted microbial therapies, and immune modulation. Ongoing research aims to clarify the mechanisms at play, personalize treatments, and harness the full power of the gut microbiome in the fight against autoimmunity.
Limitations in current research include incomplete mechanistic understanding, difficulty in translating findings from animal models to humans, and variability between individuals. Nevertheless, the interplay between the microbiome and autoimmunity is now recognized as a cornerstone of modern immunology, likely to shape the future of prevention and treatment strategies for a wide range of autoimmune diseases.